The post-pandemic era Medicaid unwinding has been an unprecedented undertaking for Medicaid enrollees, the state agency that oversees Medicaid, health care providers, and health care advocates. The unwinding process highlighted long-standing patterns within the program and offered a wealth of data to the public, providing necessary insights that can help make health care more accessible in the future.
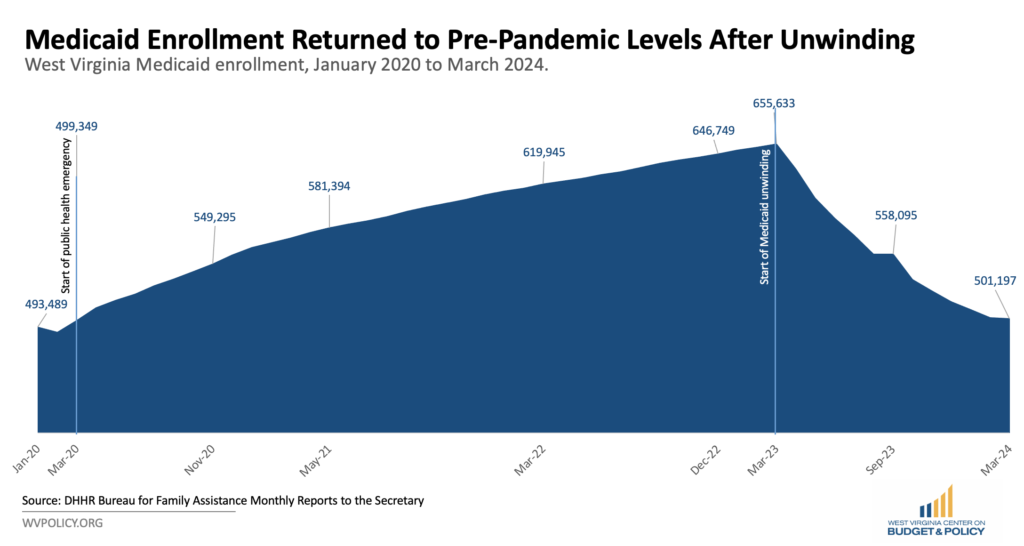
The unwinding period required the state to redetermine the eligibility of all Medicaid enrollees. Because of the pandemic-era continuous coverage requirement—and the economic downturn that made more people eligible—the Medicaid program grew significantly during the public health emergency. In January 2020, before the pandemic, West Virginia Medicaid covered roughly 493,000 people. Coverage peaked in March 2023—the last month before the continuous coverage provision ended—at about 655,500 people. By March 2024, West Virginia had roughly 500,000 people enrolled in Medicaid—a reduction of over 150,000 people—returning to pre-pandemic levels of enrollment.
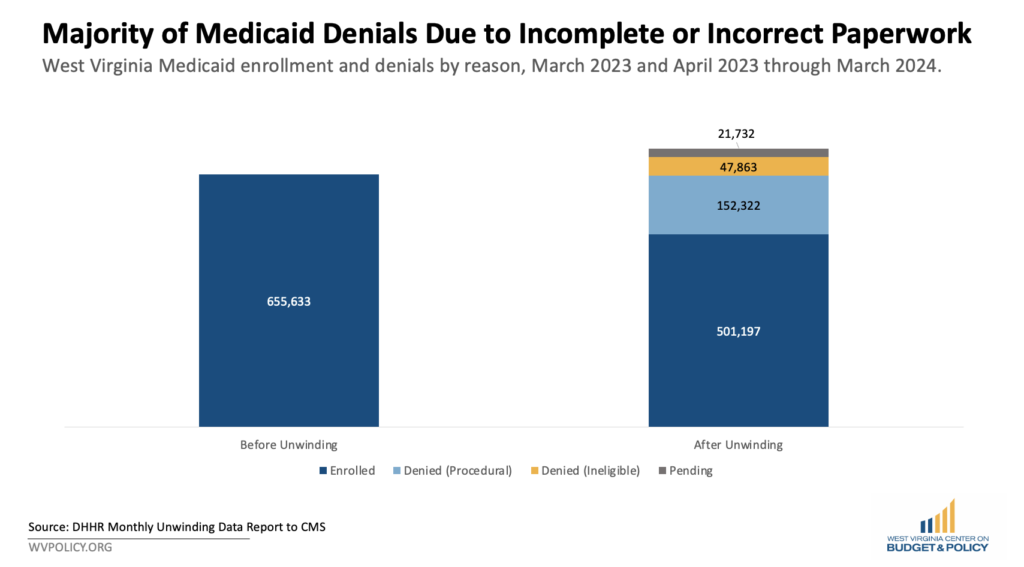
Over the last year, West Virginia has been a leader in releasing detailed information about the unwinding process and its impacts on individuals, families, and children. The state reviewed eligibility for roughly 516,000 people and about half of them, or 258,000, retained coverage. Roughly 207,600 people—a quarter of them children—lost coverage and 47,800 were found to be ineligible for Medicaid or the Children’s Health Insurance Program (CHIP). This group captures those who completed their renewal forms, most of whom were found to be over the income threshold for the program. The remainder of denials, over 150,000, were procedural denials. This refers to those who lost coverage simply because they didn’t complete a step in the renewal process, not because they were actually determined to be ineligible.
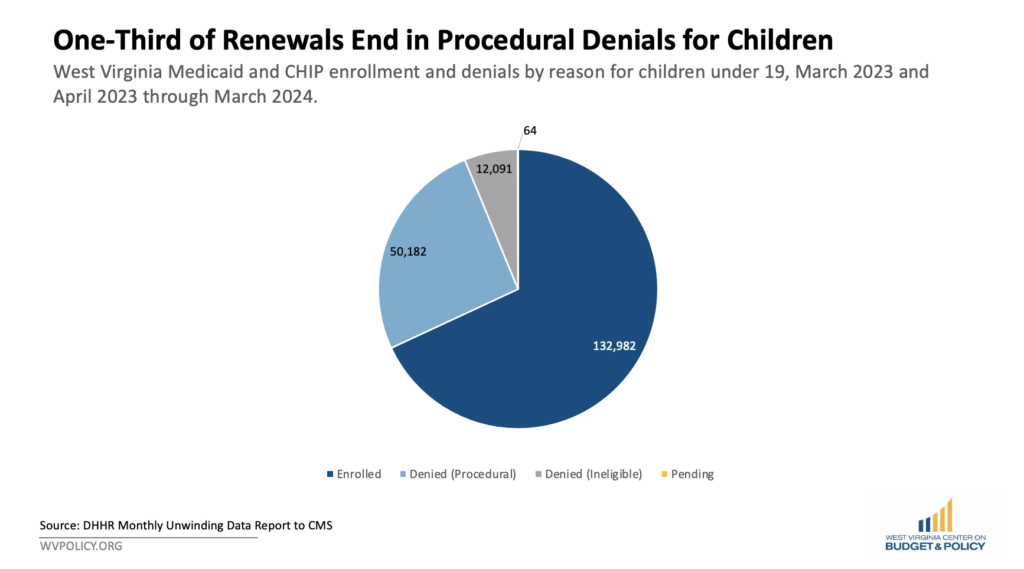
The unwinding also impacted children’s health insurance coverage. Despite being subjected to a higher income eligibility threshold than adults due to CHIP eligibility guidelines, the data showed similar patterns across both populations. West Virginia reviewed about 195,000 child enrollees for renewal. While 133,000 retained Medicaid or CHIP, about 62,000 lost coverage. Of those that lost coverage, only 12,000 were determined to be ineligible. The majority of the denials were procedural.
While the unwinding is nearing completion, the lessons learned from this period apply to ongoing Medicaid operations. West Virginia policymakers can and must address the state’s high rate of procedural denials. This figure indicates a need to help eligible families remain enrolled. One way to address this is by increasing the number of ex parte, or automatic, renewals. Ex parte renewals utilize available state and federal data sources to confirm income eligibility for enrollees and reduce bureaucratic and paperwork burdens that often confuse eligible people. This creates less paperwork for both enrollees and agency employees while still providing accurate, up-to-date information.
While some people West Virginia procedurally denied may have been over the income eligibility threshold, research suggests that most people in this category may still be within the requirements to remain covered by Medicaid. During the unwinding, while over 200,000 people lost coverage during the redetermination process, net Medicaid enrollment declined by 150,000 people, suggesting about one in four of those who lost their coverage eventually reenrolled in Medicaid or CHIP and were likely always eligible.
Several barriers can make correctly completing and returning paperwork on time onerous for enrollees, including limited access to transportation and broadband, avoidance due to anticipated hardship, and experiencing difficulty getting questions answered via phone. These barriers have serious health consequences. People who incorrectly lose Medicaid may believe they are no longer eligible and remain uninsured. Others may reapply but experience a coverage gap that leads them to delay getting care or go without needed medications. Ex parte renewals are one of West Virginia’s many options to work around these barriers. While the number of ex parte renewals has grown significantly in recent months, there is still room to increase impact.
It is also critical that West Virginia continue to share detailed enrollment and renewal data beyond the unwinding. These data highlighted long-standing patterns that need a proactive response.
Policymakers should also prioritize education and outreach about available health care programs including the Affordable Care Act (ACA) Marketplaces, Medicaid, and CHIP. Currently, there is not much state or national data available about whether those who lost coverage during the unwinding have successfully transitioned to other health coverage. An April survey conducted by the Kaiser Family Foundation showed that about 23 percent of those who were disenrolled during the unwinding period are still uninsured, with three-fourths of those who lost Medicaid reporting they worry about their health. Through robust education and outreach, West Virginia policymakers can ensure that the unwinding does not lead to a longer-term spike in the state’s uninsured rate, which could reduce health, increase hospital uncompensated care, and harm families.
Lastly, legislators must fully fund the Medicaid program. As health care costs continue to increase in the United States, West Virginia Medicaid has maintained a flat budget. And while the additional pandemic-era federal funds helped fill gaps created by years of underfunding, those funds expired at the end of the public health emergency. Now, the state must address this hole in the budget and create sustainable revenue sources to ensure the wellness of West Virginia families. By utilizing every available resource, the state can reduce procedural denials and help West Virginians remain healthy.