Infant and maternal health outcomes are just two of many factors indicating the overall health of West Virginia. They create a narrative about connections with health and communal care and indicate areas for improvement. Over the past several years, the data around infant and maternal mortality have lagged in West Virginia, making it difficult to fully understand the challenges the state faces. The West Virginia Legislature, with recommendations from health care providers and advocates, passed new legislation to address this problem. An updated law now requires more timely reports and allows the review team to interview families of deceased infants or mothers, a best practice that can offer more detailed and nuanced information. Moving forward, West Virginians will have access to more robust data that can drive important policy decisions and make the state a healthier place to live.
Each year, the Fatality and Mortality Review Team (FMRT), a multidisciplinary team created to oversee and coordinate the examination, review, and assessment of special cases of death, is required to publish an annual report concerning cases reviewed that year. Within the FMRT, an Infant and Maternal Mortality Review Panel (IMMRP) studies infant and maternal mortalities, which “require extensive studies to enable the development of strategies to reduce such deaths in the future.” The IMMRP is tasked with identifying infant and maternal death cases; reviewing relevant medical records and other data; determining the preventability of deaths; establishing trends, patterns, and risk factors; and making recommendations to policymakers, among other responsibilities.
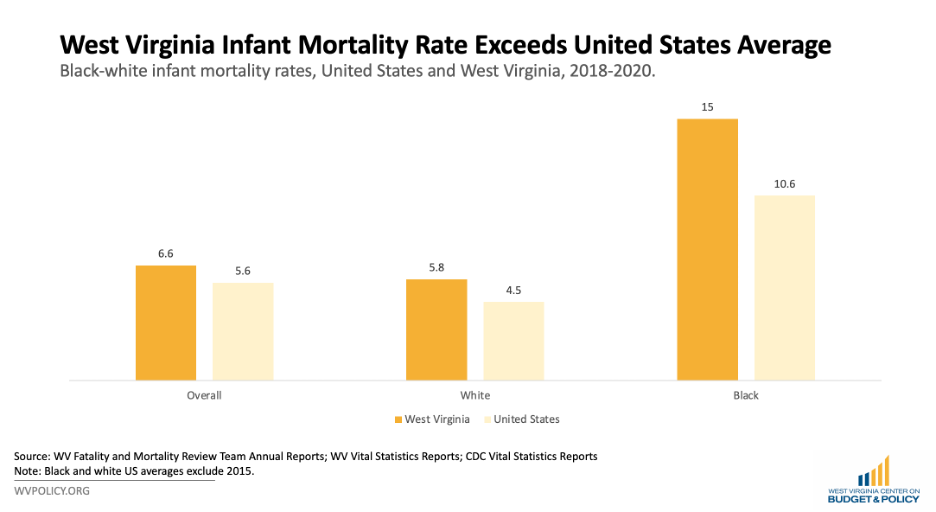
The 2023 annual report covers infant deaths between 2018 and 2020. The infant mortality rate indicates the number of children under one year who die per 1,000 live births. Between 2018 and 2020, West Virginia’s average infant mortality rate was 6.6 deaths per 1,000, a decrease from 7.2 deaths per 1,000 between 2014 and 2017. Taking a deeper look at the state data, the white infant mortality rate decreased from 6.8 deaths between 2014 and 2017 to 5.8 deaths between 2018 to 2020, respectively; over the same period, the Black infant mortality rate jumped from 13.7 to 15.0 deaths.
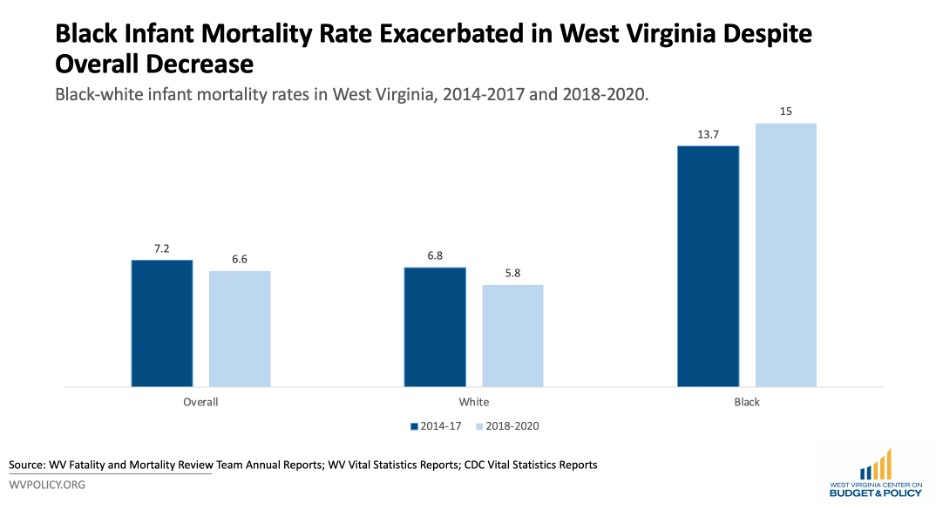
While the overall infant mortality rate decreased, the racial disparity between white and Black infants widened in West Virginia—a trend worth investigating. Furthermore, West Virginia still maintains a higher infant mortality rate than the United States overall.
The IMMRP also offered details about when and how infants passed away during this period. One in three deaths occurred before an infant was a day old, while 32 percent were between one and 28 days and the remaining 32 percent were between 29 and 365 days.
While the panel did not break out the cause of death by age, research has indicated that deaths of children who are less than one month old are more likely to stem from premature birth and low birth weight, maternal complications, and bacterial sepsis than deaths of older infants. For infants aged one day to one year, the leading causes of death are sudden infant death syndrome (SIDS) and circulatory system diseases. These deaths are mostly medical.
Indeed, in the majority of cases analyzed, the IMMRP indicated that medical conditions were the top causes of death, from prematurity to congenital malformations. The undetermined deaths were ones that the panel could not distinguish between injury and medical causes.
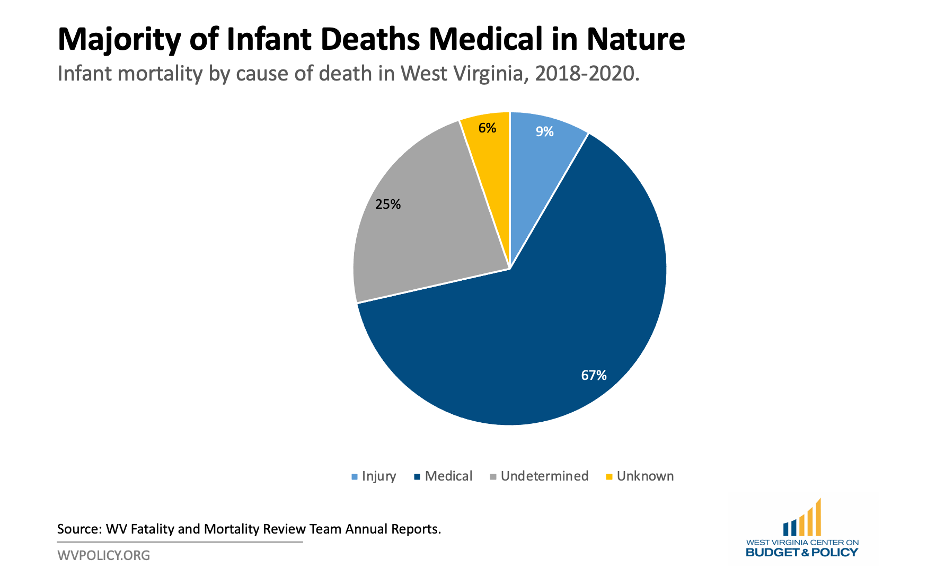
Overall, the FMRT report indicates that between 2018 and 2020, one in four infant deaths were preventable. Nearly all of these deaths were accidental or undetermined, and many—preventable or not—were sleep-related.
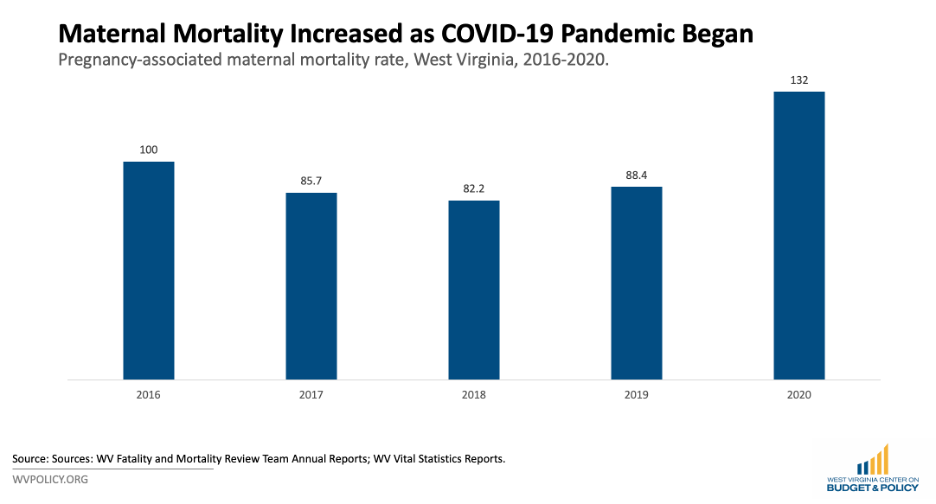
The FMRT annual report also included maternal mortality data for 2020. The maternal mortality rate measures the number of maternal deaths related to or associated with pregnancy per 100,000 live births. While pregnancy-associated deaths measure all maternal deaths that occur within this period, pregnancy-related deaths measure those aggravated by pregnancy; both measure deaths throughout pregnancy and the year afterward. The IMMRP must meet to determine the latter category, which reflects the public health standard for measuring maternal deaths. As such, the figures below reflect pregnancy-associated deaths for the time being. We included previous years’ pregnancy-associated maternal mortality rates for the sake of having a multiyear comparison. However, without more data, it is impossible to compare these data to national figures.
Still, this data provides meaningful information. In 2016, the pregnancy-associated maternal mortality rate was 100 deaths per 100,000. The rate decreased over the next few years, but jumped back to 132 deaths per 100,000 in 2020 when the COVID-19 pandemic began.
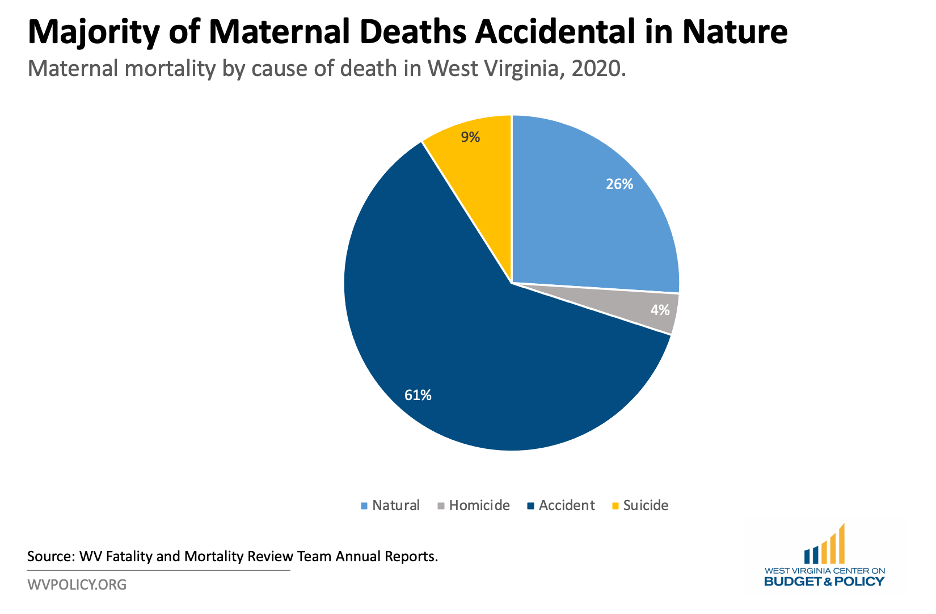
As with infant deaths, the IMMRP also reviewed maternal deaths to determine causes. Three in five maternal deaths were accidental and included factors like injuries and drug use. The natural deaths were medical, including sepsis and heart and liver conditions. It is unclear how many of these deaths were preventable.
The COVID-19 pandemic disrupted health outcomes in myriad ways, from decreased access to the health care system to increased isolation which played a major role in maternal health outcomes. The Kaiser Family Foundation conducted a study that concluded that the COVID-19 pandemic had a direct relationship with worsened mental health and increased substance use. Indeed, the most recent report from the West Virginia Office of the Chief Medical Examiner highlighted a jump in overdose deaths in the state in 2020. Between 2016 and 2019, the average number of overdose deaths was 926 deaths per year; in 2020, the figure jumped nearly 50 percent and the state lost over 1,300 people to overdoses. While it is unclear how many of these deaths were those of mothers, in a state with historically fraught mental health systems and an ongoing opioid crisis, this data may help explain the jump in maternal deaths in 2020.
These data are critical to understanding infant and maternal health outcomes in West Virginia. However, the information still lags, and without it, researchers cannot observe the full impact of the COVID-19 pandemic, recent policy changes, and other factors that played a significant role in individuals’ ability to engage meaningfully with the health care system and their community. Moving forward, these state reports will be timelier and more detailed, including the potential for family interviews. For the time being, infant and maternal health outcomes must be prioritized in West Virginia. The state must support policies that advance health care for all, ensuring that West Virginia is a safe and healthy place to live and thrive.
Join us Friday, July 26 at noon for a webinar diving deeper into this topic. Register here. We hope to see you soon!