Medicaid is a federal-state partnership that provides health coverage to over 500,000 West Virginians on average. The program is vital to West Virginia’s hospitals and providers, with research showing Medicaid expansion has resulted in reduced uncompensated care, increases in hospital operating margins, and decreases in closures of hospitals and obstetric units. Medicaid improves hospital finances by extending coverage to patients who would otherwise be uninsured and require hospital charity or uncompensated care. State Medicaid officials have warned that the program faces a $100 million shortfall in FY 2024 [1] and a $114 million shortfall in FY 2025. However, it’s important to note that the gap is primarily not a result of needed new spending but a return to pre-pandemic state budget spending. Any reduction in state spending for Medicaid, whether caused by failing to meet current spending needs or by reducing services or enrollment, would negatively impact providers and the state’s economy.
Thanks to the federal match, we receive almost three dollars in federal funds for every dollar the state invests in Medicaid. This dynamic means that while the state’s share of Medicaid is a budget expenditure, Medicaid is a source of positive revenue for West Virginia, generating far more in federal dollars than the state spends each year. Additionally, Medicaid drives jobs in the Mountain State. According to research from West Virginia University’s Bureau for Business and Economic Research, a loss of $100 million in state funds for Medicaid would cost an estimated 5,200 jobs and nearly $500 million annually in Gross Domestic Product (GDP).
During the COVID-era Public Health Emergency, the federal government increased its share of funding for Medicaid from 2020 through the end of 2023, providing an additional federal infusion of $706 million just from the increased match rate. As a result, the state saved money it typically would have spent on Medicaid out of the state budget during that period. In FYs 2020- 2023, the state’s share of Medicaid spent out of the base budget (including general revenue and lottery expenditures) was nearly $100 million less per year than it had been before the pandemic, even with increased Medicaid enrollment due to the public health emergency’s continuous coverage requirements. After adjusting for inflation, the state budget expenditures for Medicaid this year are around $250 million less than before the pandemic.
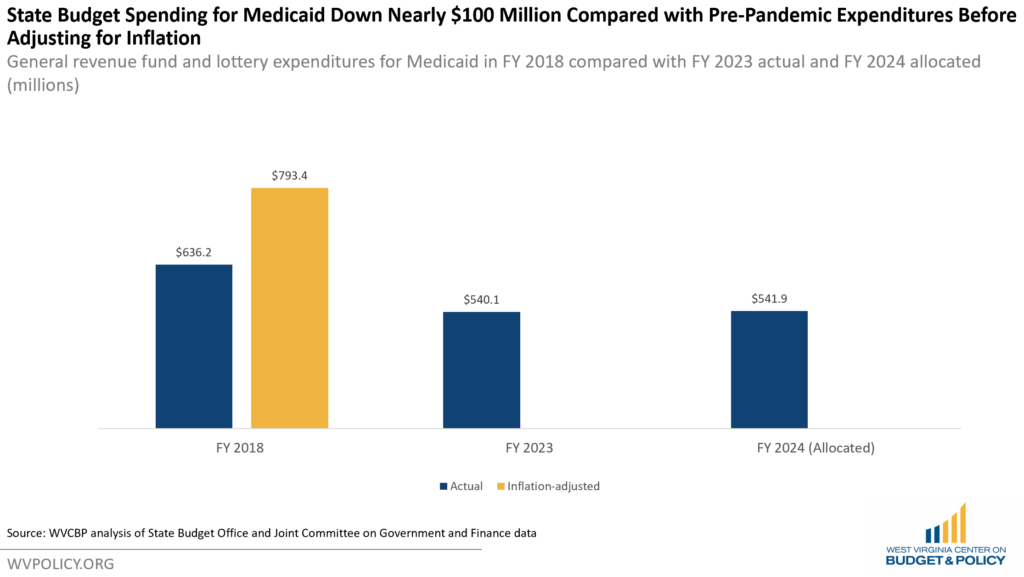
Medicaid officials have noted that the shortfall is driven by multiple factors, with the reduction in the federal match due to the end of the COVID-19 public health emergency, increasing prescription drug costs, and a possibility that total enrollment will be slightly higher than pre-pandemic enrollment all playing a role. Another factor is policymakers’ actions to use the Medicaid Trust Fund to balance other parts of the state budget in recent years, which accelerated a shortfall due to underfunding that was coming even before the pandemic.
Of all those factors, the most significant driver of the so-called shortfall is the return to pre-pandemic state match—something officials always knew would come with the end of the federal public health emergency. Senate Finance Chairman Tarr acknowledged the state’s responsibility to return to pre-pandemic Medicaid state costs earlier this year as a reason not to support Governor Justice’s costlier tax cut plan, saying “when the [increased] Medicaid FMAP goes away because of the federal COVID stuff, we end up with $152 million deficit in Medicaid”. At the time, he referred to this as funding critical to our state’s needs.
While Medicaid officials have proposed an increase in the Managed Care Organization (MCO) tax to raise additional funds for the FY 2025 shortfall, that likely doesn’t address the need in the current year, nor does it provide enough revenue to cover a long-standing Medicaid administrative budget shortfall or additional proposed provider reimbursement rates to serve vulnerable populations. Additionally, it does not reduce the responsibility of state policymakers to prioritize health care for West Virginians and our community health centers by investing state budget dollars into the program at a rate commensurate with pre-pandemic expenditures.
[1] Medicaid officials shared that they anticipate a FY 2024 shortfall of $100 million in state funding at the October WVAHC Medicaid Summit and in subsequent phone conversations with author.