After months of preparation by the state’s health agency, advocates, and other stakeholders, the COVID-19 continuous coverage rules keeping many children enrolled in Medicaid and the Children’s Health Insurance Program (CHIP) ended in April 2023. Between April 2023 and April 2024, the state must unwind (or redetermine eligibility for) all Medicaid enrollees and remove ineligible people from the rolls. In March 2023, just over 650,000 West Virginians received health insurance via Medicaid—and over a third (or 246,800) were children.
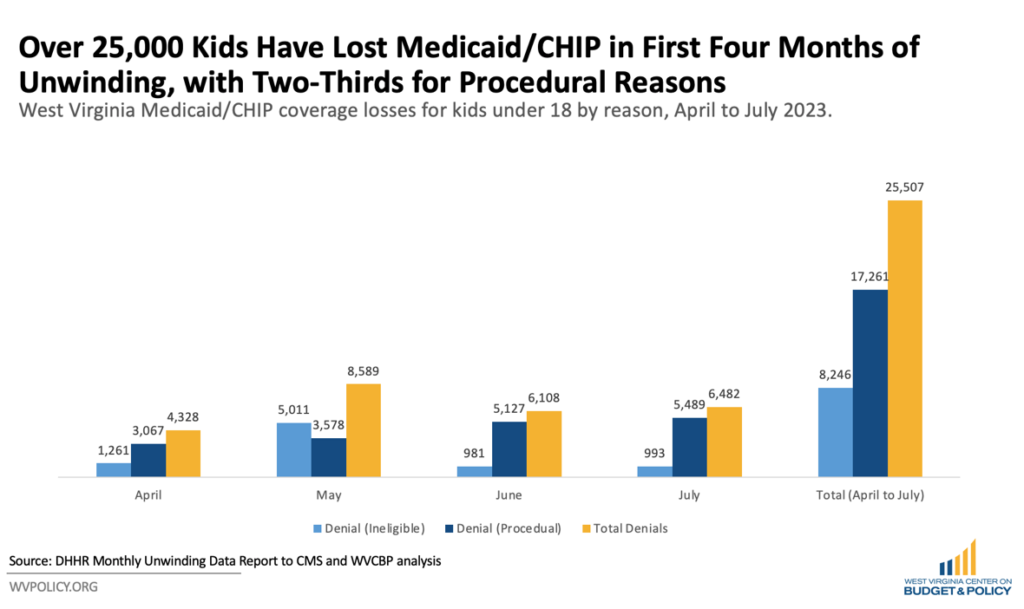
In the first four months of the long-anticipated unwinding, roughly 85,500 West Virginians have lost Medicaid or CHIP, nearly a third of whom, 25,500, are children under 18. Of the 25,500 kids who have lost coverage, two-thirds were procedural denials— meaning they lost coverage due to paperwork barriers rather than being determined ineligible. Data from the state’s health agency show that some months saw over four in five kids’ denials attributed to procedural reasons.
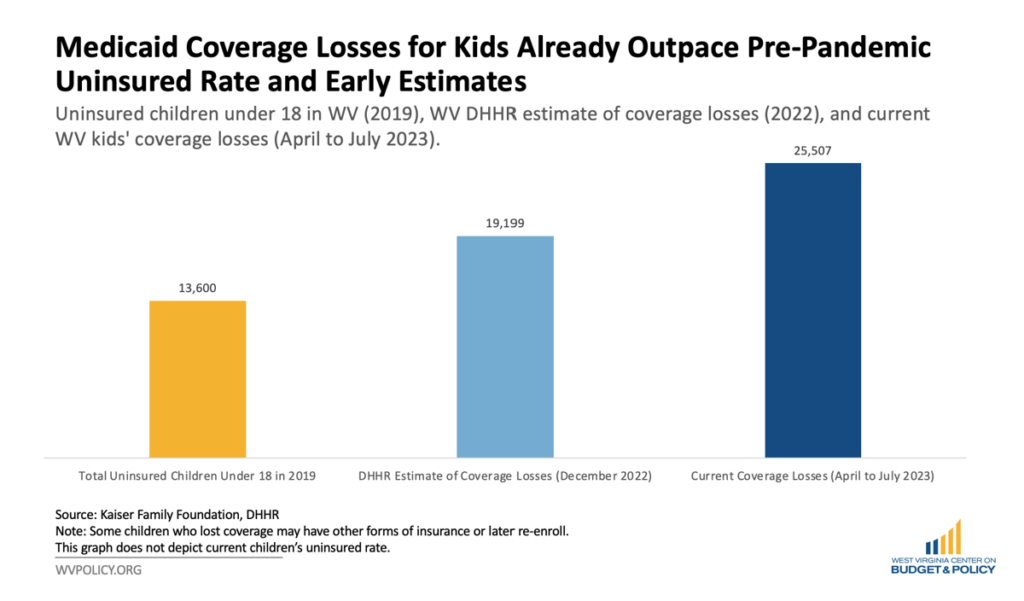
The state has already surpassed its own estimates of total child coverage losses approximately one-third of the way through the unwinding, with ten percent of kids enrolled in Medicaid or CHIP losing their health insurance. In December 2022, the Department of Health and Human Resources (DHHR) estimated that just over 19,000 kids were at risk of losing coverage, nearly a fifth of all child enrollees.[1] Without additional mitigation efforts and supports dedicated to directing to other coverage options—including employer-based or Marketplace insurance—the uninsured rate for West Virginia children could more than double its pre-pandemic rate. While it is unlikely to reach such levels, the state will probably experience an increase in uninsured kids throughout and beyond the unwinding period.
While advocates and experts long anticipated that many families, including those with children, would lose Medicaid coverage during the unwinding, it’s worth parsing out the two main denial buckets these folks may fall into: the first is because they no longer qualify, most likely because, while they qualified when they enrolled, their incomes are above the program’s income threshold; the second is because, while they might still be eligible, they did not correctly complete and submit their renewal paperwork by the requested deadline. This second category, referred to above as procedural denials, is of particular concern because many in that category are still eligible for Medicaid, cutting them off from access to necessary health care.
Medicaid has significantly prevented and treated many health issues in a state with long-standing and deep health inequities. West Virginia has prioritized ensuring that children have robust access to health care, with nearly 97 percent of kids under 18 reportedly having health insurance in 2021. Medicaid and CHIP accounted for almost 50 percent of kids’ coverage during that time.
The state is just one-third of the way through the unwinding period. With four months of redetermination data available, policymakers and advocates can course correct to mitigate coverage losses for eligible populations for the remainder of the unwinding period.
It is unclear how many children who’ve lost coverage have transitioned to other forms of insurance or re-enrolled in Medicaid/CHIP if eligible because the data is not available in real-time. Before the pandemic, the Centers for Medicaid and Medicare Services found that over a third of people who lost their Medicaid coverage returned to the program, while many others simply went uninsured. This data indicates that many will experience a lapse in coverage, at least in the short term. There are several strategies that the state can adopt to reduce the number of procedural denials, helping more kids and families stay connected to care.
Increasing the rate of administrative, or ex parte, renewals is one way West Virginia can significantly reduce the number of kids losing coverage during the unwinding and beyond. Ex parte renewalsrely on data that DHHR already has access to—such as tax information, quarterly wage data, unemployment, and other sources—to confirm eligibility and automatically renew qualified Medicaid participants who have adequate income information on file. This policy will allow the agency to spend less time working on individual cases and eliminate the opportunity for many enrollees to complete and submit their paperwork incorrectly.
West Virginia has significantly increased the number of cases renewed via ex parte in recent months to just over ten percent—though it still lags behind all but eight states, including neighboring Ohio, Maryland, Kentucky, and Virginia. Increasing the rate of ex parte renewals will significantly reduce procedural denials and churn (folks rolling on and off Medicaid), increase caseworker efficiency, and improve long-term health outcomes, especially for its youngest and most vulnerable enrollees.
The Kaiser Family Foundation found that coverage affordability was the top driver determining whether individuals had health insurance. During the public health emergency, West Virginia waived CHIP premiums and copays, ensuring that children would not lose access to care because their families could not afford it. The state joined 18 others who eliminated this barrier to care throughout the emergency, including six that do not plan to reinstate them. Waiving CHIP premiums and copays throughout the unwinding period can help ease the transition from Medicaid for many families.
Lastly, targeting outreach efforts toward ensuring continuous coverage for children will help ensure parents and caretakers are aware of the unwinding and have all the tools necessary to renew successfully. This strategy can include efforts around the back-to-school season, sending kids who receive free or reduced lunch home with flyers, and other targeted means of ensuring families with children stay connected to care.
While the nation is just partway through the Medicaid unwind, these early insights can help mitigate unnecessary coverage losses, especially among vulnerable populations like children. Reducing procedural denials will be meaningful to many families and create a healthier state for its children.
If you have a child who has lost their Medicaid or CHIP coverage since April, we want to hear from you about your experience and transition to other health coverage. Contact Alex at agallo@wvpolicy.org or 304-720-8682.
[1] Email to author from DHHR representative, Anita Hayes, Dec. 2, 2022.