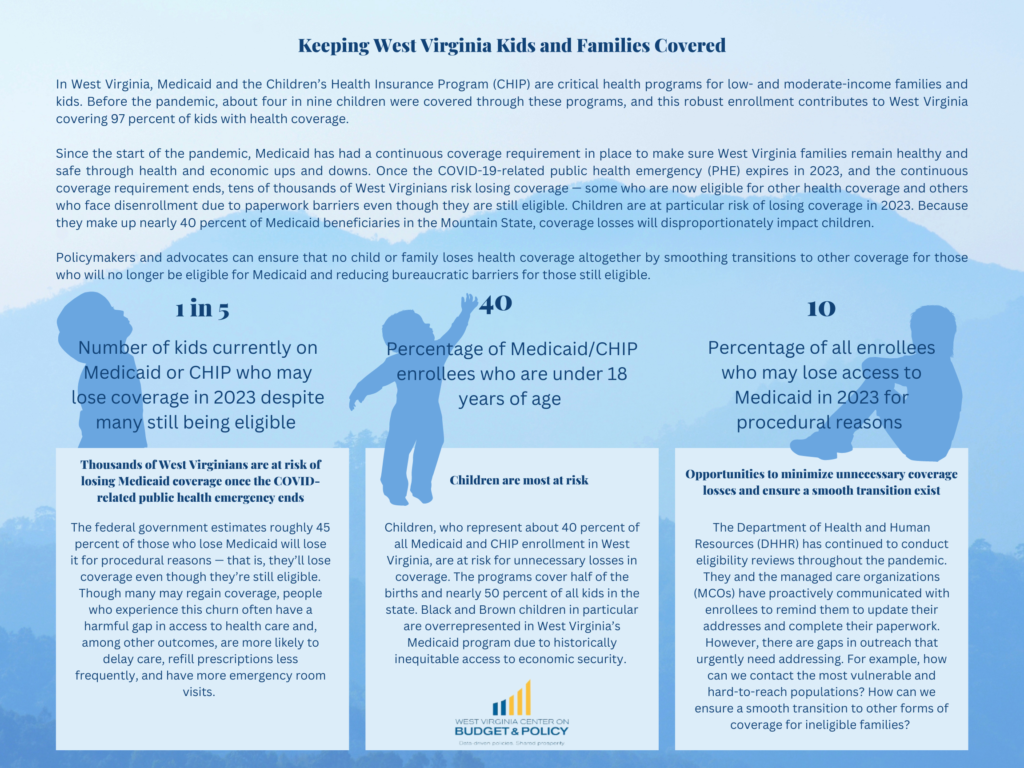
In West Virginia, Medicaid and the Children’s Health Insurance Program (CHIP) are critical health programs for low- and moderate-income families and kids. Before the pandemic, about four in nine children were covered through these programs, and this robust enrollment contributes to West Virginia covering 97 percent of kids with health coverage.
Since the start of the pandemic, Medicaid has had a continuous coverage requirement in place to make sure West Virginia families remain healthy and safe through health and economic ups and downs. Once the COVID-19-related public health emergency (PHE) expires in 2023, and the continuous coverage requirement ends, tens of thousands of West Virginians risk losing coverage – some who are now eligible for other health coverage and others who face disenrollment due to paperwork barriers even though they are still eligible. Children are at particular risk of losing coverage in 2023. Because they make up nearly 40 percent of Medicaid beneficiaries in the Mountain State, coverage losses will disproportionately impact children.
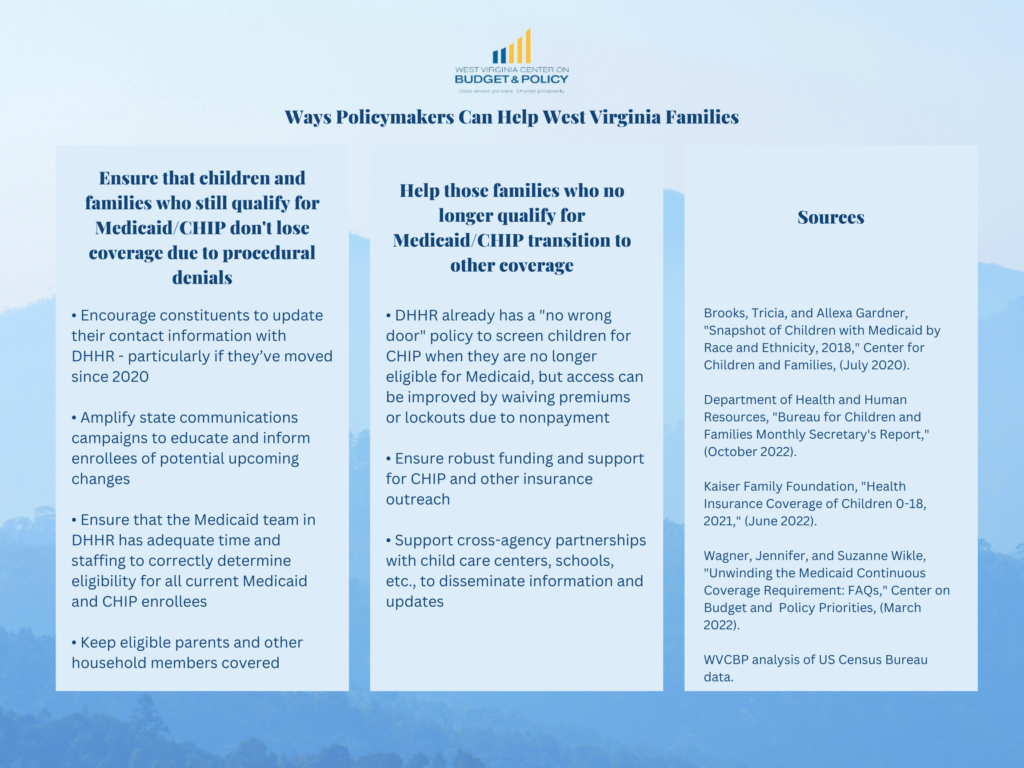
Policymakers and advocates can ensure that no child or family loses health coverage altogether by smoothing transitions to other coverage for those who will no longer be eligible for Medicaid and reducing bureaucratic barriers for those still eligible.