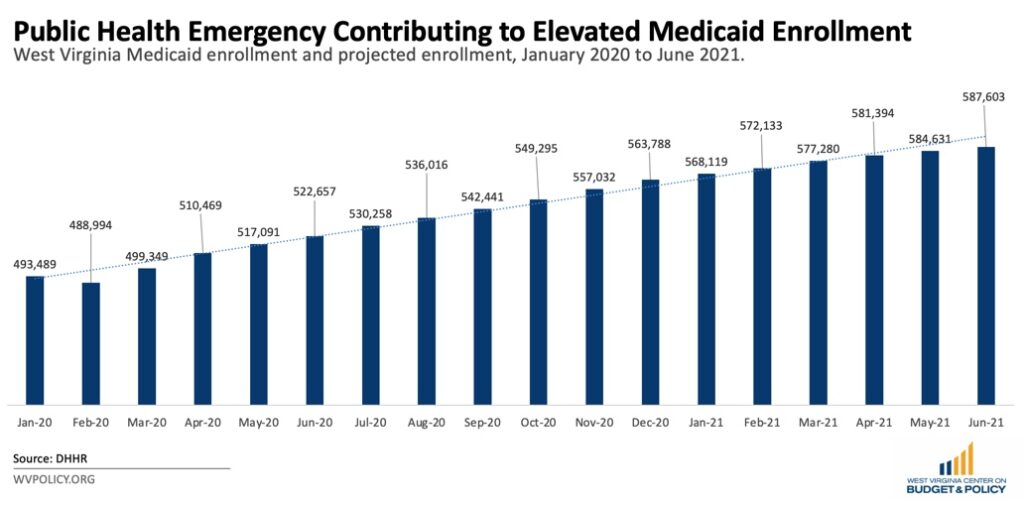
Medicaid enrollment has increased, both nationally and in West Virginia, in response to the COVID-19 pandemic. Recent data show enrollment increased in the Mountain State from its pre-pandemic baseline of 489,000 individuals in February 2020 to 587,000 people in June 2021. The reasons for this are twofold: first, unprecedented pandemic-related job losses, which peaked at nearly 16 percent in April 2020, made many more people eligible for Medicaid. Second, the Families First Coronavirus Response Act included a continuous coverage requirement that prohibited state Medicaid agencies from disenrolling people through the public health emergency (PHE). Even as the economy continues to recover, the continuous coverage requirement will contribute to ongoing high enrollment through the PHE. This provision was critical to ensuring that West Virginians had continuous health coverage throughout the pandemic and could continue to access regular health services during challenging economic times.
The Centers for Medicare & Medicaid Services (CMS) highlighted that, due to the pandemic, over 80 million people across the country are enrolled in Medicaid and CHIP. Experts expect this figure to increase through the PHE, which could end as early as mid-January 2022. In a typical month prior to the pandemic, Medicaid would experience significant churn or people falling off of the program’s rolls; however, the PHE and accompanying continuous coverage requirement halted that. As a result, everyone who has been enrolled in Medicaid since March 2020 is still enrolled today – and will be through the PHE. Experts anticipate that Medicaid enrollment will continue to grow before the unwinding process eventually begins.
Decisions made during the remainder of the PHE can significantly improve the continuity of care for West Virginia’s Medicaid enrollees and the stability of state finances during 2022. CMS issued guidance outlining its flexibilities for returning the Medicaid program to normal once the PHE ends, including a year for state agencies to evaluate eligibility. Despite this guidance, the Urban Institute predicts that Medicaid enrollment could decrease by about 15 million people nationally, representing nearly one-fifth of overall current enrollment figures. They also estimate that most of those folks will qualify for coverage elsewhere in the insurance market – one-third could receive affordable subsidized coverage through the Marketplace, while the remainder would likely have access to private insurance through an employer. Experts also anticipate that many children will lose Medicaid coverage, although at a lower rate than adults. Nationally, 60 percent of children who could lose Medicaid coverage at the end of the PHE could become eligible for CHIP, and that percentage could be higher in West Virginia.
While these figures offer a promising glimpse into life after the PHE, there are several opportunities for both the federal and state governments to ensure that as few eligible folks lose health care coverage as possible during the transition. Two policies that could help West Virginia mitigate the consequences of the unwinding of the PHE are conducting more ex parte renewals and ensuring that folks enrolled in Medicaid update their contact information.
West Virginia can more efficiently unwind the PHE by conducting more ex parte renewals or renewals that employ existing data to automatically re-enroll eligible Medicaid enrollees. The state has access to income data for many Medicaid enrollees through Workforce WV’s unemployment portal, payroll data, eligibility verifications for other programs that the Department of Health and Human Resources (DHHR) manages, and other means. Utilizing that data to renew eligible enrollees automatically would save staff time and improve the Medicaid experience for users. Despite this being an available tool, fewer than 25 percent of renewals in West Virginia utilize this streamlining option. Several states, including Alabama, Arkansas, and Ohio, have reported ex parte renewal rates exceeding 75 percent, resulting in fewer people losing coverage. Employing this type of renewal could more quickly verify critical information and minimize the number of eligible people unnecessarily losing coverage as the state unwinds the PHE.
Another critical part of ensuring continuous coverage is contacting enrollees about necessary and pertinent information, including the need to complete renewal forms. During the pandemic, many people have moved, making mail notices a less effective means of reaching them. While the state has not yet begun to send renewal forms to Medicaid enrollees, that will be a central part of unwinding the PHE – especially if they do not implement ex parte renewals ahead of that period. Missed notices could exacerbate the number of eligible individuals and families losing coverage as the PHE ends since they would not be made aware of vital information.
Implementing ex parte renewals and ensuring that enrollees update their contact information are just two of several ways to prepare for the unwinding of the PHE so that as few West Virginians as possible lose health care coverage. Acting proactively ahead of the end of the PHE will contribute to a healthier state beyond the pandemic.